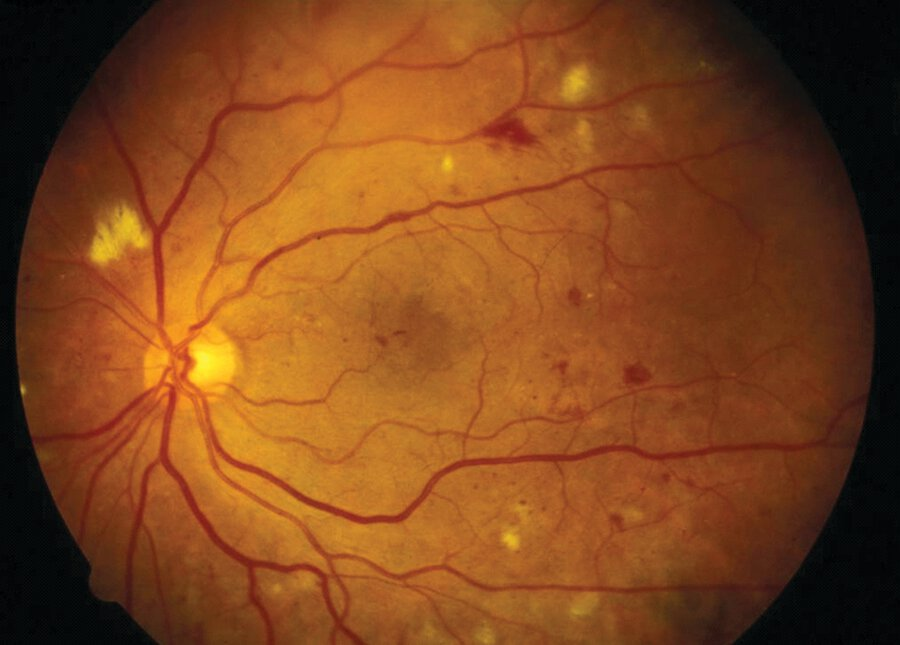
Diabetic Retinopathy
Presentation :
- Leading cause of preventable blindness among persons with diabetes between ages 20 and 74 years in developed countries
Pathophysiology :
- Diabetic retinopathy changes are classified as nonproliferative or proliferative:
- Nonproliferative: findings may include microaneurysms, dot and blot hemorrhages, hard exudates (lipid deposition), soft exudates or cotton-wool spots (ischemic superficial nerve fibers), venous bleeding, and intraretinal microvascular abnormalities.
- Proliferative: characterized by neovascularization 2/2 chronic ischemia which may result in vitreous hemorrhage, retinal detachment, and vision loss

- Macular edema causes vision loss and may occur with nonproliferative and proliferative retinopathy
Diagnostic Testing:
Treatment :
- Control of blood glucose and blood pressure (BP)
- Macular edema: intraocular injection of anti-VEGF agents (eg, ranibizumab, bevacizumab, aflibercept) and/or focal laser photocoagulation.
- Intraocular corticosteroids can be used to treat persistent macular edemna
- High-risk or complicated proliferative retinopathy: anti-VEGF drugs, panretinal laser photocoagulation and sometimes vitrectomy
- High-risk characteristics include: vitreous hemorrhage, extensive preretinal neovascularization, or anterior segment neovascularization/neovascular glaucoma
- Anti-VEGF therapy requires monthly injections for at least 12 months followed by intermittent injections to prevent recurrent macular edema.
- Vitrectomy can help preserve and often restore lost vision in patients with any of the following:
- Persistent vitreous hemorrhage
- Extensive preretinal membrane formation
- Traction retinal detachment
- Recalcitrant diabetic macular edema
Prognosis:
References:
Created on: Friday 11-08-2023