Hypercalcemia
Presentation :
- Painful bones, renal stones, porcelain thrones (polyuria), abdominal groans (abd pain), psychic moans/psychiatric overtones
- Hypercalcemia usually does not have a huge impact on EKG; common findings include:
- Shortened QT
- Bundle branch block.
- AV block with bradyasystolic arrest at extremely high levels.
- ST elevation may rarely be seen.
Pathophysiology :
- Thiazide diuretics may cause mild hypercalcemia
- Hypercalcemia associated with lithium therapy is caused by altered PTH secretion and may occur years after initiation of therapy
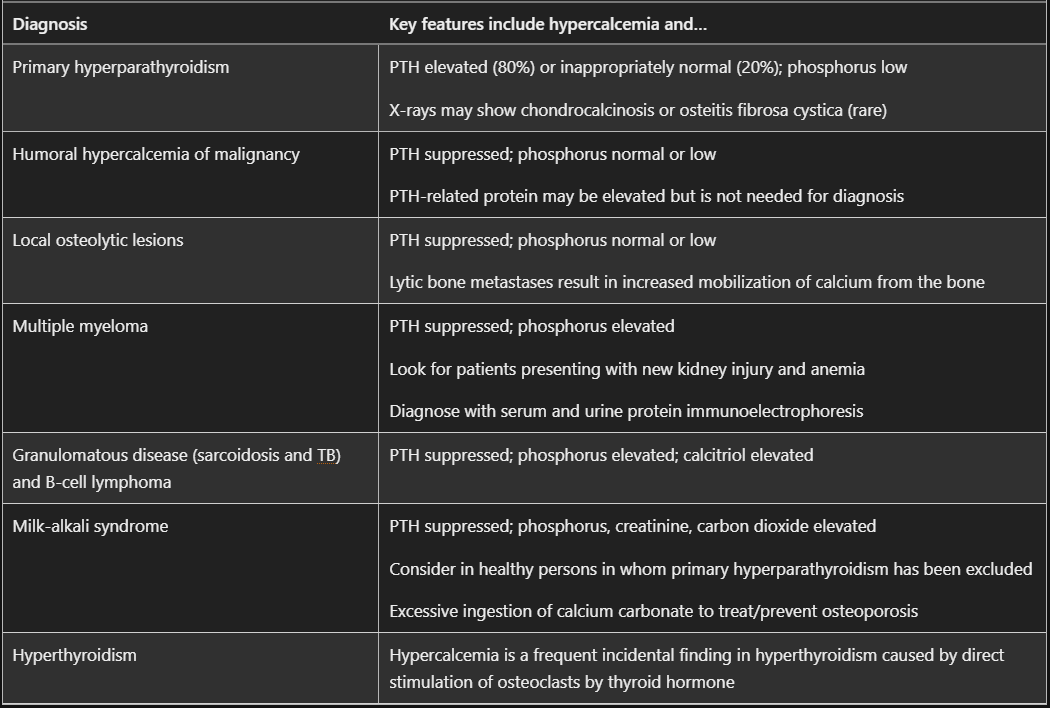
- Primary hyperparathyroidism is the most common cause of hypercalcemia in outpatients and is most commonly caused by a solitary Parathyroid Adenoma
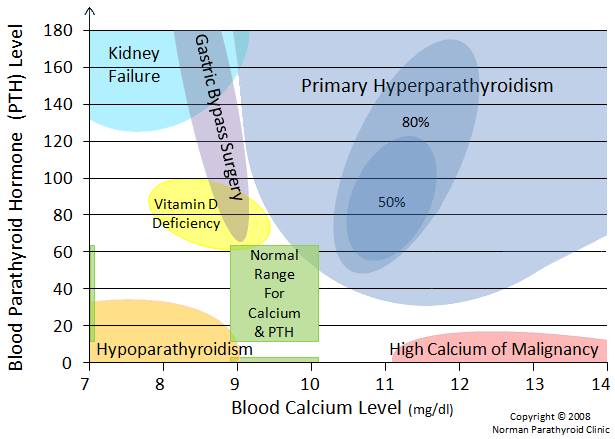
- PTH Mediated Hypercalcemia
- Primary Hyperparathyroidism: resulting from Parathyroid Adenoma, Parathyroid Carcinoma, and Parathyroid Hyperplasia
- Tertiary Hyperparathyroidism
- Familial Hypocalciuric Hypercalcemia
- Non–PTH-Mediated Hypercalcemia
- Hypercalcemia of Malignancy
- Vitamin D–Dependent Hypercalcemia
- Vitamin D Intoxication
- Granulomatous Disease: Unregulated conversion of 25-Vit D to 1,25-Vit D in granulomas 2/2 fungal infection, tuberculosis, sarcoidosis, and lymphoma
- Sarcoidosis may be associated with hypercalcemia (10% of patients) and hypercalciuria (50% of patients).
- Milk-Alkali Syndrome: Ingestion of large amounts of calcium, typically from antacid use (e.g., calcium carbonate), especially with coexistent chronic kidney disease, causes milk-alkali syndrome.
Diagnostic Testing:
- When hypercalcemia is incidentally noted, next check ionized calcium (iCa; more accurately reflects physiologically active calcium levels).
- Can use albumin to correct serum total calcium for a proxy, but there is some evidence that this is not particularly accurate and a poor substitute for iCa
- Calcium corrected for albumin = Serum total calcium + 0.8 * [Normal Albumin (4) - Serum Albumin]
- Can use albumin to correct serum total calcium for a proxy, but there is some evidence that this is not particularly accurate and a poor substitute for iCa
- If hypercalcemia is confirmed, simultaneous measurement of serum calcium and PTH is the next step in categorizing PTH-mediated and non–PTH-mediated hypercalcemia.
-
Also helpful to measure phos, Cr, and 25-Vit D.
-
PTH secretion decreases abruptly in response to an increase in serum calcium concentration. Therefore, a PTH level that is elevated or inappropriately normal (usually in the upper half of the reference range) is diagnostic of PTH-mediated hypercalcemia.
AAFP Algorithm: (source)
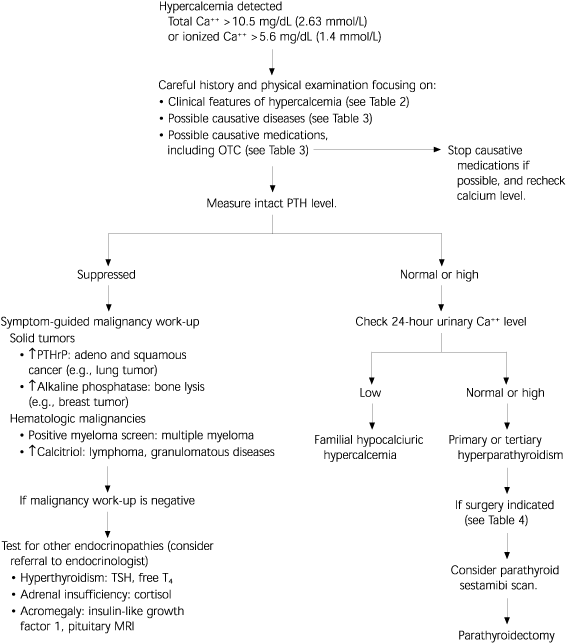
Medications include: Thiazides (usually mild hyperCa), Lithium, Calcium antacids (milk-alkali), Vit A intoxication (including from topicals), Vit D excess, Teriparatide, TPN, Rebound after denosumab discontinuation
-
Treatment :
- Treatment of underlying condition, see above #Pathophysiology
- Generally speaking can lower calcium using a combination of:
- IV fluids (hypercalcemia typically causes volume depletion due to enhanced fluid excretion by the kidneys and reduced oral intake)
- Plasmalyte may be the optimal fluid as it is a balanced crystalloid that contains low levels of calcium
- Lactated ringers is suboptimal because it contains calcium. However, LR has a physiological concentration of calcium (1.35 mM), which will be lower than the patient's calcium concentration. Thus, LR will will not elevate the patient's calcium level, so LR remains safe to use in patients with hypercalcemia.
- Normal saline is often suboptimal because it causes Non-Anion Gap Metabolic Acidosis (NAGMA) (and many patients with hypercalcemia will have pre-existing acidosis).
- Calcitonin
- Typically reserved for severe hypercalcemia
- Causes significant but only temporary reduction in calcium due to tachyphylaxis
- Works by reducing reabsorption of calcium from bone and reducing renal calcium reabsorption
- Usual dose: 4 units/kg SubQ q12h
- Intranasal administration is ineffective
- May cause localized injection site reaction
- Consider testing for calcitonin allergy in those with known allergy to fish or significant atopy
- Calcitonin is salmon-derived and can cause skin reactions to anaphylaxis
- Calcitonin can potentially lower serum lithium levels
- Bisphosphonates
- Appear to work regardless of the etiology of hypercalcemia by preventing resorption of calcium from bones (except as noted below)
- Delayed onset (days) so should be started early, using calcitonin and IVF to temporize while waiting
- Contraindications:
- Hypercalcemia from Milk-alkalai syndrome; should improve with removal of provoking ingestant
- Caution is needed for premenopausal women, as bisphosphonates may become incorporated into bone and released during a subsequent pregnancy.
- Renal failure (depending on the agent).
- Zoledronate (Zometa) is the preferred agent
- The main side-effect of concern is renal failure. The risk of inducing clinically significant renal failure from a single dose of zoledronic acid is very low. Nonetheless, among patients with pre-existing renal dysfunction, the following measures should be considered to reduce the risk of kidney injury:
- (a) Dose-reduction:(31826272)
- GFR 50-60 ml/min: 3.5 mg
- GFR 40-49 ml/min: 3.3 mg
- GFR <39 ml/min: 3 mg
- (b) Infuse over a longer duration of time (e.g., 60 minutes).
- (c) Ensure that the patient is adequately volume resuscitated prior to administration.
- (d) Avoid other nephrotoxic agents
- (a) Dose-reduction:(31826272)
- The main side-effect of concern is renal failure. The risk of inducing clinically significant renal failure from a single dose of zoledronic acid is very low. Nonetheless, among patients with pre-existing renal dysfunction, the following measures should be considered to reduce the risk of kidney injury:
- IV fluids (hypercalcemia typically causes volume depletion due to enhanced fluid excretion by the kidneys and reduced oral intake)
References:
- https://www.aafp.org/pubs/afp/issues/2003/0501/p1959.html
- https://emcrit.org/ibcc/hypercalcemia/
- Kenny, Colin M., et al. "Things We Do for No Reason™: Calculating a “Corrected Calcium” Level." Journal of Hospital Medicine 16.8 (2021): 499-501.
- MKSAP
Created on: Friday 08-11-2023