Invasive Aspergillosis
Presentation :
- Invasive aspergillosis most often occurs in immunosuppressed patients with neutropenia or who are hematopoietic stem cell transplant recipients.
- Most common site is pulmonary (60%), but sinusitis, brain abscess, and disseminated infection may also occur.
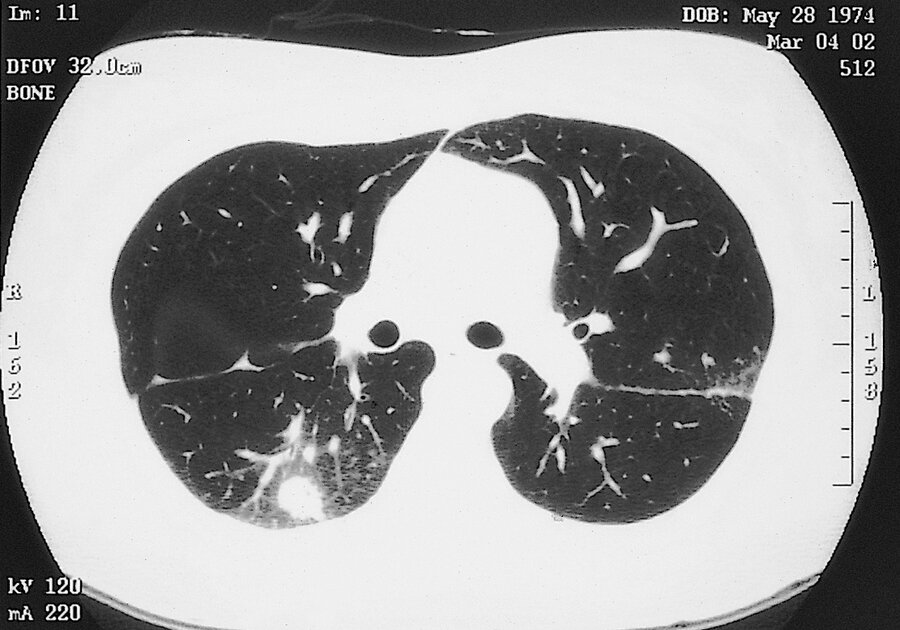
- CT chest can reveal septic emboli (nodules, often with a “halo sign”; ) (Figure 19), thromboembolic pulmonary infarction (wedge-shaped peripheral densities), or necrosis with cavitation (air-crescent sign) are typical findings
- “Halo sign,” is an area of low attenuation surrounding a pulmonary nodule that reflects hemorrhage into the adjacent tissues.
Pathophysiology :
- Aspergillus fumigatus is the most common species causing disease in humans, followed by A. flavus, A. niger, and the amphotericin-resistant A. terreus.
- Aspergillus produces disease after inhalation of airborne spores (90%) and occasionally by traumatic skin inoculation.
- Aspergillosis usually begins in the respiratory tract and then enters the circulatory system (angioinvasion).
Diagnostic Testing:
- Blood culture results are generally negative
- Serum Galactomannan testing
- If invasive pulmonary aspergillosis is suspected, bronchoscopy, bronchoalveolar lavage, and, if possible, tissue biopsy are recommended to establish the diagnosis
- Methenamine silver stain reveals septate hyaline hyphae with dichotomous acute angle (45°) branching.

Treatment :
- First-line treatment of invasive aspergillosis is voriconazole
- Alternative agents include liposomal amphotericin B, isavuconazole, or other lipid formulations of amphotericin B.
- When possible, reversing immunosuppression improves treatment response.
Prognosis:
References:
Created at: periodic/daily/August/2023-08-01-Tuesday