Renal Tubular Acidosis (RTA)
Presentation :
- Usually asymptomatic
- Nephrolithiasis and nephrocalcinosis are possible, particularly with type 1 RTA.
- Signs of extracellular fluid volume depletion may develop from urinary water loss accompanying electrolyte excretion in type 2 RTA.
- People with type 1 or type 2 RTA may show symptoms and signs of hypokalemia, including muscle weakness, hyporeflexia, and paralysis. Bony involvement (eg, bone pain and osteomalacia in adults and rickets in children) may occur in type 2 and sometimes in type 1 RTA.
- Type 4 RTA is usually asymptomatic with only mild acidosis, but cardiac arrhythmias or paralysis may develop if hyperkalemia is severe.
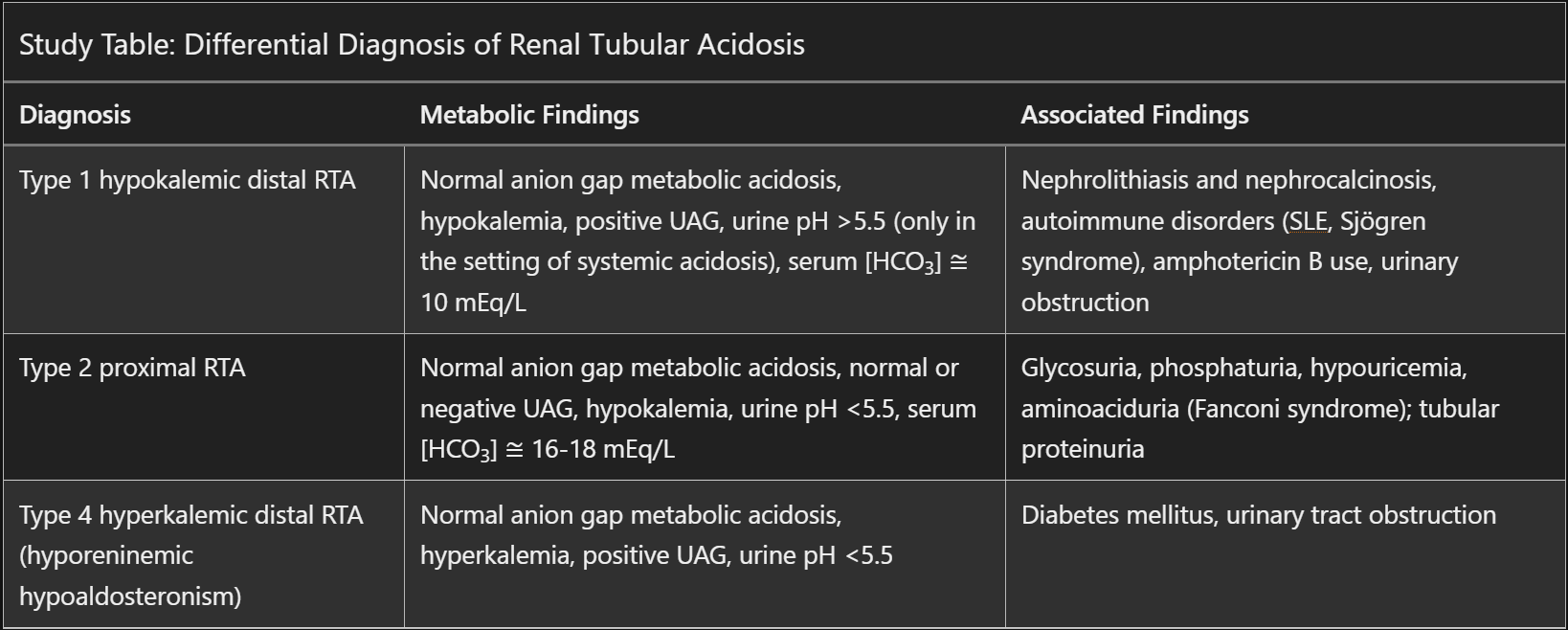
- Non-anion gap metabolic acidosis
Pathophysiology :
- Type 2:
- Results from inadequate bicarb resorption in the proximal tubule
- Usually accompanied by other evidence of proximal tubular dysfunction, including complete or partial Fanconi syndrome (glycosuria, phosphaturia, aminoaciduria, hypouricemia)
- Because the distal nephron functions appropriately, urine can still be acidified to a pH <5.5 and NH4+ production will be normal, usually making the urine anion gap negative.
- Hypokalemia is also often present due to increased distal tubular potassium secretion. This occurs because sodium accompanies bicarbonate to the distal tubule, where sodium is reabsorbed in exchange for potassium.
- The most common causes include myeloma light chains as well as nephrotoxic medications such as ifosfamide, carbonic anhydrase inhibitors (acetazolamide and topiramate), and tenofovir disoproxil fumarate (although toxicity is much less likely with tenofovir alafenamide).
- Type 1 + 4:
- Inability of the kidney to adequately excrete acid
- Type 1:
- Distal tubular defect results in impaired excretion of hydrogen ions (hence, low urine ammonium and positive urine anion gap) with inability to acidify urine below a pH of 6.0.
- Urinary potassium wasting in the setting of diminished proton secretion underlies the development of hypokalemia
- Most common causes include Sjögren syndrome and other tubulointerstitial diseases, including reflux uropathy and obstructive uropathy
- Can also be caused by medications such as amphotericin B and lithium
- Hypercalciuria and hyperphosphatemia are frequent in untreated type 1 RTA because of increased calcium and phosphate release from bone due to buffering of acid
- Reduced tubular calcium resorption in the context of acidosis exacerbates hypercalciuria.
- Increased proximal reabsorption of citrate in the context of acidosis and hypokalemia causes hypocitraturia. Citrate usually inhibits calcium crystallization; therefore, hypocitraturia, in addition to hypercalciuria, increases the risk for calcium phosphate stones and nephrocalcinosis.
- Type 4:
- Caused by aldosterone deficiency or resistance
- Primary adrenal insufficiency (Addison disease) may cause aldosterone deficiency.
- Hyporeninemic hypoaldosteronism is a more common cause and may occur in the presence of various kidney diseases, most often diabetic kidney disease.
- Aldosterone resistance can occur in those with tubulointerstitial disease, including urinary obstruction, sickle cell disease, medullary cystic kidney disease, and kidney transplant rejection.
- Numerous drugs can reduce aldosterone production, including ACE inhibitors, angiotensin receptor blockers, direct renin inhibitors, heparin, and cyclooxygenase-2 inhibitors.
- Decrease aldosterone activity leads to increased K+ rea
- Caused by aldosterone deficiency or resistance
Diagnostic Testing:
-
Type 1: confirmed by a urine pH that remains > 5.5 during systemic acidosis. The acidosis may occur spontaneously or be induced by an acid load test (administration of ammonium chloride 100 mg/kg orally). Normal kidneys reduce urine pH to < 5.2 within 6 hours of acidosis.
-
Type 2: diagnosed by measurement of the urine pH and fractional bicarbonate excretion during a bicarbonate infusion (sodium bicarbonate 0.5 to 1.0 mEq/kg/hour [0.5 to 1.0 mmol/L] IV). In type 2, urine pH rises above 7.5, and the fractional excretion of bicarbonate is > 15%. Because IV bicarbonate can contribute to hypokalemia, potassium supplements should be given in adequate amounts before infusion.
-
Type 4: confirmed by a history of a condition that could be associated with type 4 RTA, chronically elevated potassium, and normal or mildly decreased bicarbonate. In most cases plasma renin activity is low, aldosterone concentration is low, and cortisol is normal.
-
Urine anion gap is used as a surrogate to assess kidney acid excretion and differentiate between RTAs (given NH4+ is hard to measure directly)
-
Urine Anion Gap = (Urine Sodium + Urine Potassium) – Urine Chloride
- Ammonium cation excretion results in proportionately less excretion of sodium and potassium (the predominant urine cations).
- Chloride anion excretion continues with ammonium cation excretion to maintain electrical neutrality.
-
Decreased urine NH4+ production, results in a positive urine anion gap
-
Increased urine NH4+ production, results in a negative urine anion gap
Treatment :
- Type 2:
- Correction of acidemia with bicarbonate therapy
- Addition of a low-dose thiazide diuretic may help by inducing volume depletion, lowering the GFR, and thereby decreasing the filtered load of bicarbonate
- Addition of a potassium-sparing diuretic may limit the degree of renal potassium wasting.
- Type 1:,
- Administration of sodium bicarbonate/sodium citrate usually corrects the metabolic acidosis.
- Type 4: RTA, the primary goal of therapy is to correct the hyperkalemia, which will treat the acid-base disturbance. These patients, often with early CKD and diabetes, may develop severe hyperkalemia following treatment with ACE inhibitors or ARBs.
Prognosis:
References: